Neglected Tropical Diseases in Africa: A Persistent Public Health Challenge
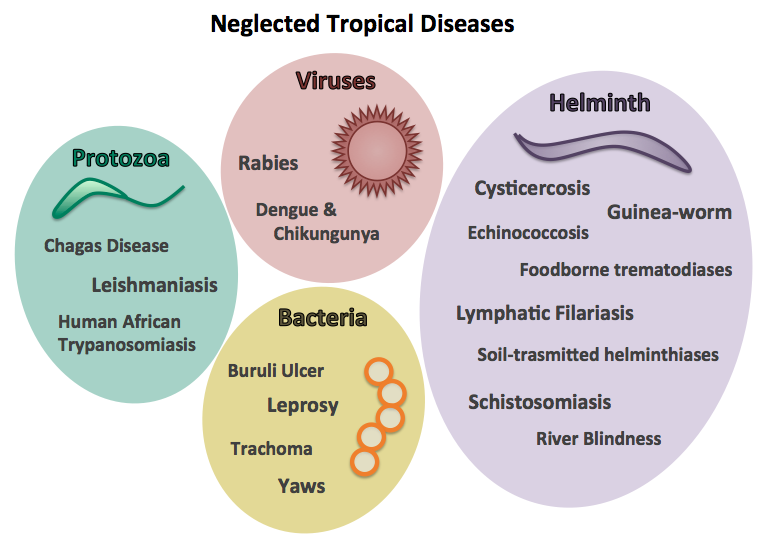
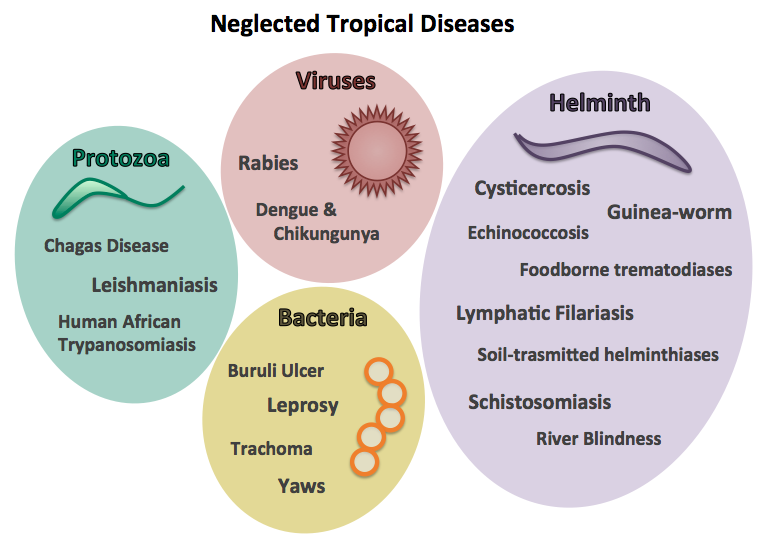
Neglected Tropical Diseases (NTDs) represent a group of communicable diseases that disproportionately affect impoverished populations in tropical and subtropical regions. These diseases lead to chronic health issues, disabilities, and economic hardships, perpetuating the cycle of poverty. In Africa, NTDs are a significant public health concern, with the continent bearing a substantial portion of the global burden.
NTDs encompass a variety of diseases, including but not limited to lymphatic filariasis (elephantiasis), onchocerciasis (river blindness), schistosomiasis (bilharzia), trachoma, and soil-transmitted helminthiases (intestinal worms). These diseases cause severe pain, disability, and social stigma, trapping affected communities in a vicious cycle of poverty and ill health.
According to the World Health Organization (WHO), approximately 400 million people in Africa are at risk of NTDs. The economic burden is profound, with affected households losing an estimated US$33 billion annually due to healthcare costs and lost productivity. Conversely, investments in NTD prevention and treatment yield significant returns, with an estimated benefit of US$25 for every US$1 invested.
Kenya, like many other African nations, faces a significant burden from NTDs. The country is endemic to 19 of the 20 WHO-recognized NTDs, with approximately 25 million Kenyans affected. The most prevalent NTDs in Kenya include:
Beyond Kenya, other African nations also face significant challenges with NTDs:
Lymphatic filariasis, commonly known as elephantiasis, is caused by parasitic worms transmitted through mosquito bites. The disease leads to severe swelling of the limbs and genitals, resulting in disability and social exclusion. In Africa, millions are affected, with Kenya’s coastal regions, Nigeria, and Mozambique being major hotspots.
In 2021, Kenya launched mass drug administration campaigns in endemic counties such as Kilifi, Kwale, and Mombasa. Nigeria has also conducted large-scale MDA programs, covering millions of at-risk individuals.
Onchocerciasis, or river blindness, is caused by the parasitic worm Onchocerca volvulus, transmitted by blackflies. The disease can result in severe itching, skin lesions, and blindness. Approximately 99% of onchocerciasis cases occur in Africa, with over 85 million people living in endemic areas.
Nigeria, Cameroon, and Uganda have implemented ivermectin treatment programs to control the disease. Uganda, in particular, has made remarkable progress in eliminating transmission in several regions.
Schistosomiasis is a parasitic disease caused by Schistosoma species, transmitted through contact with contaminated freshwater. As of 2021, over 250 million people worldwide were affected, with sub-Saharan Africa accounting for approximately 85% of cases.
Kenya, Tanzania, and Mali have implemented school-based deworming programs, particularly in areas around freshwater lakes and rivers. Tanzania’s deworming initiatives have reached millions of children, significantly reducing the disease burden.
Trachoma is a bacterial infection caused by Chlamydia trachomatis, leading to blindness if untreated. As of June 2022, 125 million individuals globally lived in trachoma-endemic areas, with Africa being the most affected region.
Ethiopia has been a major success story, with millions receiving antibiotics and undergoing surgeries to prevent blindness. South Sudan has also made progress in eliminating trachoma through sustained health interventions.
Several African countries have developed National Master Plans for the Elimination of NTDs, including Kenya, Nigeria, and Ethiopia. These plans include:
Africa has made notable strides in combating NTDs. Leprosy has been nearly eliminated as a public health problem, with only the Comoros yet to achieve the elimination goal in one of its three islands. Forty-two African countries have been certified free of Guinea worm disease. Additionally, six countries have eliminated trachoma as a public health problem, and in 2022, Togo became the first African nation to eliminate four NTDs.
A remarkable example is the near-eradication of Guinea worm disease, spearheaded by former U.S. President Jimmy Carter through The Carter Center. The disease, which afflicted 3.5 million people in 20 countries in 1986, saw a reduction to just 14 cases in four African nations by 2023.
Despite progress, significant challenges persist:
Innovative solutions are being explored to enhance NTD management. In South Sudan, Médecins Sans Frontières (MSF) is testing an AI-powered app to identify snakes and improve the treatment of snakebites. Leveraging a database of 380,000 snake images, the AI can identify venomous species, aiding in the correct use of rare and costly antivenoms.
In Kenya and Nigeria, researchers are working on new diagnostic tools and vaccines for NTDs. The Kenya Medical Research Institute (KEMRI) and the Nigerian Institute of Medical Research (NIMR) are collaborating with global health agencies to develop sustainable solutions.
While Africa has made significant strides in combating NTDs, much remains to be done. Strategic planning, increased funding, and innovative research are crucial in achieving the goal of eliminating these diseases as public health threats. Strengthening community engagement, improving sanitation, and integrating NTD control into primary healthcare will be key in ensuring sustainable progress. With sustained commitment, Africa can overcome the burden of NTDs and ensure a healthier future for all.